Learning how to draw blood is a crucial skill for nurses. This in-depth guide, brought to you by LEARNS.EDU.VN, will provide a detailed, step-by-step explanation of the venipuncture process, covering everything from identifying the correct veins to mastering best practices for patient safety and accurate results. Whether you’re a nursing student, a new nurse, or an experienced professional looking to refine your technique, this resource will empower you with the knowledge and confidence to excel in phlebotomy. We will also explore common challenges and solutions, ensuring you are well-prepared for any situation.
1. Understanding the Importance of Phlebotomy Skills for Nurses
Phlebotomy, the process of drawing blood, is a fundamental skill for nurses, playing a vital role in patient care and diagnostic accuracy. Nurses proficient in venipuncture can contribute significantly to efficient healthcare delivery and improve patient outcomes.
- Diagnostic Testing: Blood samples are essential for a wide range of diagnostic tests, providing crucial information about a patient’s health status.
- Treatment Monitoring: Regular blood draws are necessary to monitor the effectiveness of treatments and adjust medication dosages as needed.
- Patient Safety: Skilled phlebotomy minimizes patient discomfort and reduces the risk of complications such as hematoma or infection.
- Timely Results: Nurses who can efficiently draw blood can expedite the diagnostic process, leading to quicker treatment decisions.
- Increased Efficiency: Proficiency in phlebotomy allows nurses to contribute to a smoother workflow in various healthcare settings.
2. Foundational Knowledge: Anatomy and Physiology for Venipuncture
A solid understanding of the relevant anatomy and physiology is essential for successful and safe venipuncture. Nurses must be familiar with the major veins in the arm and hand, as well as the underlying structures to avoid complications.
2.1. Key Veins for Venipuncture
- Median Cubital Vein: Located in the antecubital fossa (the bend of the elbow), this is often the first choice due to its large size and accessibility.
- Cephalic Vein: Located on the thumb side of the arm, it is another common site, especially when the median cubital vein is not suitable.
- Basilic Vein: Located on the pinky side of the arm, it is often a last resort due to its proximity to the brachial artery and median nerve.
2.2. Underlying Structures to Avoid
- Brachial Artery: Located deep within the arm, puncture can cause significant bleeding and nerve damage.
- Median Nerve: Located close to the basilic vein, injury can lead to pain, numbness, and loss of function.
- Tendons: Superficial and easily avoided with proper technique.
2.3. Vein Selection Criteria
- Size: Choose a vein that is large enough to accommodate the needle size.
- Accessibility: Select a vein that is easily visible and palpable.
- Location: Avoid areas with scarring, hematomas, or other abnormalities.
- Condition: Select a vein that is healthy and free from inflammation or irritation.
3. Essential Equipment and Supplies for Blood Collection
Having the right equipment readily available is crucial for a smooth and efficient blood draw. Nurses should be familiar with each item and its purpose.
3.1. Common Phlebotomy Supplies
| Supply | Purpose |
|---|---|
| Evacuated Collection Tubes | Collect blood samples for specific laboratory tests |
| Needles (various gauges) | Penetrate the vein to draw blood |
| Needle Holder (Vacutainer) | Securely holds the collection tube and needle |
| Tourniquet | Restricts blood flow to make veins more prominent |
| Alcohol Swabs | Disinfect the venipuncture site |
| Gauze Pads | Apply pressure to the puncture site after needle removal |
| Adhesive Bandage | Cover and protect the puncture site |
| Gloves | Protect the nurse from exposure to bloodborne pathogens |
| Sharps Container | Dispose of used needles and other sharps safely |
| Laboratory Requisition Forms | Document patient information, tests ordered, and collection details |
| Biohazard Bags | Transport blood samples to the laboratory |
3.2. Choosing the Right Needle Gauge
Needle gauge refers to the diameter of the needle. A higher gauge number indicates a smaller needle.
- 21-23 Gauge Needles: Commonly used for routine venipuncture.
- 25 Gauge Needles: May be used for patients with small or fragile veins, but blood flow may be slower.
- Larger Gauge Needles (16-18 Gauge): Typically used for blood donation or rapid blood draws.
3.3. Understanding Blood Collection Tubes
Different blood collection tubes contain specific additives that are required for different laboratory tests. It’s essential to use the correct tube for each test to ensure accurate results.
| Tube Color | Additive(s) | Common Tests |
|---|---|---|
| Red | None or Clot Activator | Chemistry, Serology, Immunology |
| Lavender | EDTA | Complete Blood Count (CBC), Hemoglobin A1c |
| Light Blue | Sodium Citrate | Coagulation Studies (PT, PTT, INR) |
| Green | Heparin (Sodium, Lithium, Ammonium) | Chemistry (e.g., Ammonia, Electrolytes) |
| Gray | Sodium Fluoride, Potassium Oxalate | Glucose, Lactate |
| Yellow | ACD Solution A or B | DNA Studies, Paternity Testing |
4. Step-by-Step Guide to Performing Venipuncture
Mastering the technique of venipuncture requires practice and attention to detail. Here is a comprehensive step-by-step guide:
4.1. Preparation
- Gather Supplies: Collect all necessary equipment and supplies.
- Verify Orders: Check the laboratory requisition form and confirm the tests ordered with the patient.
- Identify Patient: Use two patient identifiers (e.g., name and date of birth) to ensure correct patient identification, as mandated by JCAHO.
- Explain Procedure: Explain the procedure to the patient and answer any questions.
- Check Allergies: Ask the patient about any allergies to antiseptics, adhesives, or latex.
- Position Patient: Position the patient comfortably in a chair or lying down.
- Hand Hygiene: Perform thorough hand hygiene using soap and water or an alcohol-based hand sanitizer.
- Don Gloves: Put on clean gloves.
4.2. Vein Selection and Preparation
- Apply Tourniquet: Apply the tourniquet 3-4 inches above the intended puncture site. Ensure it is tight enough to restrict venous blood flow but not arterial flow.
- Palpate Vein: Palpate the veins to identify a suitable vein for puncture.
- Cleanse Site: Cleanse the venipuncture site with an alcohol swab in a circular motion, starting from the center and moving outwards. Allow the area to air dry for 30 seconds.
- Anchor Vein: Use your non-dominant hand to gently pull the skin taut below the puncture site to anchor the vein and prevent it from rolling.
4.3. Needle Insertion and Blood Collection
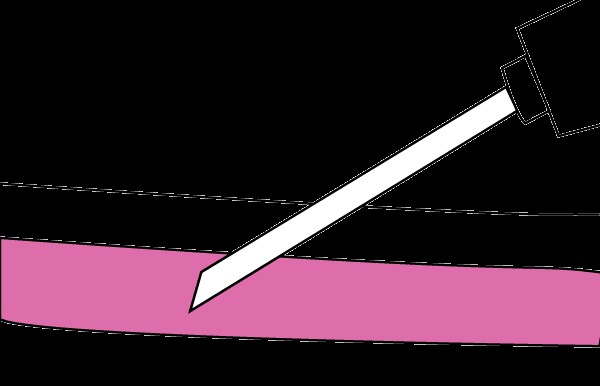
- Insert Needle: With the bevel facing up, insert the needle at a 15-30 degree angle into the vein.
- Advance Needle: Gently advance the needle a short distance into the vein until you see a flash of blood in the needle hub.
- Attach Tube: Stabilize the needle holder and gently push the evacuated tube into the holder until the needle pierces the tube stopper. Blood should begin to flow into the tube.
- Fill Tubes: Fill the tubes in the correct order of draw, as specified by the laboratory.
- Release Tourniquet: Once the last tube is filling, release the tourniquet.
- Remove Tube: Remove the last tube from the holder.
- Remove Needle: Gently remove the needle from the vein.
- Apply Pressure: Immediately apply pressure to the puncture site with a sterile gauze pad.
- Dispose of Needle: Immediately dispose of the used needle in a sharps container.
4.4. Post-Venipuncture Care
- Apply Bandage: Apply an adhesive bandage to the puncture site after the bleeding has stopped.
- Label Tubes: Label all blood collection tubes with the patient’s name, date of birth, date and time of collection, and your initials.
- Invert Tubes: Gently invert the tubes several times to mix the blood with the additives.
- Transport Specimens: Transport the blood specimens to the laboratory promptly in a biohazard bag, along with the laboratory requisition form.
- Monitor Patient: Observe the patient for any signs of bleeding or discomfort.
5. Common Challenges and Troubleshooting in Phlebotomy
Even with proper technique, nurses may encounter challenges during venipuncture. Here are some common problems and solutions:
| Challenge | Possible Cause(s) | Solution(s) |
|---|---|---|
| No Blood Flow | Needle not in vein, needle bevel against vein wall, collapsed vein, vacuum lost in tube | Gently advance or retract needle, rotate needle slightly, try a different vein, ensure tube is not expired or damaged |
| Hematoma Formation | Needle went through vein, insufficient pressure after needle removal, bleeding disorder | Apply firm pressure for at least 5 minutes, elevate arm, apply ice pack, assess patient for bleeding disorders |
| Rolling Vein | Vein not anchored properly, excessive movement by patient | Anchor vein more firmly, ask patient to remain still, use a smaller needle |
| Collapsed Vein | Excessive vacuum, fragile veins, tourniquet too tight | Use a smaller tube, release tourniquet slightly, try a different vein |
| Patient Fainting/Vasovagal Syncope | Anxiety, pain, dehydration | Position patient supine, apply cold compress to forehead, monitor vital signs, provide reassurance |
| Difficult Vein Access | Dehydration, obesity, scarring, IV drug use | Use a vein finder, apply heat to area, try a different site, consult with experienced colleague, consider using a butterfly needle |
6. Best Practices for Patient Safety and Comfort
Patient safety and comfort should always be a top priority during venipuncture.
6.1. Minimizing Patient Discomfort
- Communicate Clearly: Explain the procedure and answer any questions.
- Use a Gentle Approach: Avoid jerky movements and be mindful of the patient’s comfort level.
- Apply Topical Anesthetic: Consider using a topical anesthetic cream or spray for patients with anxiety or sensitive skin.
- Distraction Techniques: Engage the patient in conversation or offer a distraction during the procedure.
6.2. Preventing Infections
- Hand Hygiene: Perform thorough hand hygiene before and after the procedure.
- Sterile Technique: Use sterile equipment and maintain a sterile field.
- Skin Antisepsis: Cleanse the venipuncture site thoroughly with an appropriate antiseptic.
- Sharps Disposal: Dispose of used needles and other sharps immediately in a designated sharps container.
6.3. Avoiding Nerve Damage
- Proper Vein Selection: Avoid the basilic vein due to its proximity to the median nerve.
- Gentle Needle Insertion: Avoid forceful or deep needle insertion.
- Patient Feedback: Pay attention to the patient’s feedback and stop immediately if they report pain, numbness, or tingling.
7. The Role of Continuing Education and Training in Phlebotomy
Phlebotomy is a skill that requires ongoing education and training to maintain proficiency and stay up-to-date with best practices.
7.1. Importance of Certification
- Demonstrates Competency: Certification validates that a nurse has met specific standards of knowledge and skill in phlebotomy.
- Enhances Credibility: Certification can increase a nurse’s credibility and employability.
- Promotes Patient Safety: Certified nurses are more likely to adhere to best practices and minimize the risk of complications.
7.2. Continuing Education Opportunities
- Workshops and Seminars: Attend workshops and seminars to learn new techniques and review current guidelines.
- Online Courses: Take online courses to expand your knowledge and earn continuing education credits.
- Professional Organizations: Join professional organizations such as the National Phlebotomy Association (NPA) or the American Society for Clinical Pathology (ASCP) to access resources and networking opportunities.
- Hospital Training Programs: Participate in hospital-sponsored training programs to stay current with institutional policies and procedures.
7.3. Staying Updated with Current Guidelines
- World Health Organization (WHO): Consult the WHO guidelines for best practices in phlebotomy.
- Centers for Disease Control and Prevention (CDC): Review the CDC’s recommendations for infection control and prevention.
- Professional Journals: Read articles in professional journals to stay informed about the latest research and advancements in phlebotomy.
8. Ethical and Legal Considerations in Phlebotomy
Nurses performing phlebotomy must be aware of the ethical and legal considerations involved.
8.1. Patient Consent
- Informed Consent: Obtain informed consent from the patient before performing venipuncture.
- Right to Refuse: Respect the patient’s right to refuse the procedure.
- Documentation: Document the patient’s consent in the medical record.
8.2. Patient Confidentiality
- Protect Patient Information: Maintain patient confidentiality and protect their personal health information.
- HIPAA Compliance: Comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations.
8.3. Scope of Practice
- Know Your Limitations: Be aware of your scope of practice and only perform procedures that you are qualified to perform.
- Supervision: Seek supervision from a qualified healthcare professional when necessary.
8.4. Legal Liability
- Negligence: Avoid negligent acts that could harm the patient.
- Malpractice Insurance: Maintain adequate malpractice insurance coverage.
- Documentation: Maintain accurate and complete documentation of the procedure.
9. Advanced Techniques in Venipuncture
As nurses gain experience, they may encounter situations requiring advanced techniques.
9.1. Using a Butterfly Needle
- Small Veins: Butterfly needles are useful for patients with small or fragile veins.
- Elderly Patients: They are often preferred for elderly patients with thin skin and fragile veins.
- Difficult Access: Butterfly needles can be easier to maneuver in difficult-to-access areas.
9.2. Drawing Blood from a Central Line
- Sterile Technique: Strict sterile technique is essential to prevent infection.
- Flushing the Line: Flush the central line before and after drawing blood.
- Discarding Initial Sample: Discard the initial sample to avoid contamination with heparin or other medications.
9.3. Venipuncture in Pediatric Patients
- Age-Appropriate Communication: Use age-appropriate language and techniques to explain the procedure to children.
- Parental Involvement: Involve parents or caregivers to provide comfort and support.
- Smaller Needles: Use smaller needles and collection tubes.
- Distraction Techniques: Utilize distraction techniques such as toys or videos to help children remain calm.
10. The Future of Phlebotomy: Innovations and Advancements
The field of phlebotomy is constantly evolving with new innovations and advancements.
10.1. Vein Visualization Technology
- Infrared Vein Finders: These devices use infrared light to visualize veins beneath the skin, making it easier to locate and puncture veins.
- Ultrasound Guidance: Ultrasound can be used to guide needle placement, especially for patients with difficult venous access.
10.2. Point-of-Care Testing (POCT)
- Rapid Results: POCT devices allow for rapid blood testing at the patient’s bedside, providing immediate results.
- Improved Efficiency: POCT can improve efficiency and reduce turnaround time for critical laboratory tests.
10.3. Minimally Invasive Blood Collection
- Capillary Blood Sampling: Collecting blood from a finger stick or heel stick can be less invasive and more comfortable for some patients.
- Microneedle Technology: Microneedle devices are being developed to collect small amounts of blood painlessly and non-invasively.
11. LEARNS.EDU.VN: Your Partner in Nursing Education
At LEARNS.EDU.VN, we are committed to providing high-quality educational resources for nurses at all stages of their careers. Our comprehensive online platform offers a wide range of courses, articles, and resources designed to help you excel in your profession.
- Expert-Developed Content: Our content is developed by experienced nurses and healthcare professionals.
- Interactive Learning: We offer interactive learning modules, quizzes, and simulations to enhance your understanding.
- Continuing Education Credits: Earn continuing education credits to meet your professional development requirements.
- Personalized Learning Paths: Create a personalized learning path to focus on the areas that are most relevant to your career goals.
- Community Support: Connect with other nurses and healthcare professionals in our online community.
We believe that continuous learning is essential for providing the best possible patient care. Let LEARNS.EDU.VN be your partner in achieving your professional goals.
12. Embracing Lifelong Learning as a Nurse
The journey of a nurse is one of continuous learning and growth. As healthcare evolves, nurses must embrace lifelong learning to stay at the forefront of their field.
- Stay Curious: Maintain a sense of curiosity and a desire to learn new things.
- Seek Mentorship: Find a mentor who can provide guidance and support throughout your career.
- Attend Conferences: Attend professional conferences to network with colleagues and learn about the latest trends and innovations.
- Read Widely: Read professional journals, textbooks, and online resources to expand your knowledge.
- Share Your Knowledge: Share your knowledge and expertise with others by mentoring new nurses, presenting at conferences, or writing articles.
By embracing lifelong learning, nurses can enhance their skills, advance their careers, and make a meaningful difference in the lives of their patients.
13. Empowering Nurses to Provide Exceptional Care
At LEARNS.EDU.VN, we are dedicated to empowering nurses to provide exceptional care to their patients. We believe that by providing access to high-quality education, resources, and support, we can help nurses achieve their full potential and make a positive impact on the healthcare system.
- Patient-Centered Care: We emphasize the importance of patient-centered care in all of our educational materials.
- Evidence-Based Practice: We promote the use of evidence-based practice to guide clinical decision-making.
- Interprofessional Collaboration: We encourage interprofessional collaboration to improve patient outcomes.
- Quality Improvement: We provide tools and resources to support quality improvement initiatives.
- Advocacy: We advocate for nurses and the nursing profession to ensure that they have the resources and support they need to succeed.
Join us at LEARNS.EDU.VN and become part of a community of nurses who are committed to excellence in patient care.
14. Navigating Pediatric Phlebotomy: Tips for Drawing Blood from Children
Drawing blood from children requires a specialized approach that focuses on minimizing anxiety and ensuring a positive experience. Here are some essential tips:
- Preparation is Key: Explain the procedure in simple, age-appropriate terms using toys or dolls to demonstrate.
- Parental Support: Encourage a parent or caregiver to be present to provide comfort and reassurance.
- Distraction Techniques: Utilize toys, books, videos, or bubbles to distract the child during the blood draw.
- Topical Anesthetics: Apply a topical anesthetic cream or patch to the site at least 30 minutes prior to the procedure.
- Smaller Needles and Tubes: Use smaller gauge needles and pediatric-sized blood collection tubes.
- Positioning: Securely position the child to prevent movement, but avoid using excessive force. Consider having a parent hold the child in their lap.
- Positive Reinforcement: Praise the child for their cooperation and offer a small reward after the procedure.
- Honesty: Be honest with the child about any potential discomfort, but reassure them that it will be brief.
- Avoid Surprises: Never perform the blood draw without warning the child.
- Teamwork: Collaborate with other healthcare professionals to create a supportive and efficient environment.
15. Mastering the Art of Difficult Venipuncture: Strategies for Success
Some patients present unique challenges when it comes to venipuncture. Here are strategies for overcoming difficult vein access:
- Thorough Assessment: Conduct a thorough assessment to identify potential challenges such as obesity, dehydration, scarring, or collapsed veins.
- Tourniquet Placement: Experiment with tourniquet placement, trying different positions and tightness levels to enhance vein visibility.
- Warm Compress: Apply a warm compress to the area for 5-10 minutes to dilate the veins.
- Hydration: Encourage the patient to drink water prior to the procedure to improve hydration and vein volume.
- Vein Visualization: Use a vein finder or transilluminator to locate deeper or less visible veins.
- Alternative Sites: Consider alternative venipuncture sites such as the hand, wrist, or foot (with physician approval).
- Butterfly Needles: Butterfly needles can be easier to maneuver in difficult-to-access areas and are less likely to collapse fragile veins.
- Experienced Assistance: Seek assistance from an experienced colleague or phlebotomist.
- Patience: Be patient and persistent, but avoid excessive probing, which can cause pain and hematoma formation.
- Documentation: Document all attempts and the rationale for site selection in the patient’s medical record.
16. The Importance of Effective Communication in Phlebotomy
Effective communication is crucial for building trust, reducing anxiety, and ensuring a positive experience for patients undergoing venipuncture.
16.1. Building Rapport
- Introduce yourself and your role.
- Address the patient by name.
- Make eye contact and smile.
- Speak clearly and calmly.
16.2. Explaining the Procedure
- Describe the procedure in simple, non-technical terms.
- Explain the purpose of the blood draw.
- Answer any questions the patient may have.
- Address any concerns or anxieties.
16.3. Providing Reassurance
- Acknowledge the patient’s feelings.
- Reassure them that the procedure is safe and routine.
- Emphasize your commitment to minimizing discomfort.
16.4. Seeking Feedback
- Ask the patient if they have any pain or discomfort during the procedure.
- Encourage them to communicate any concerns or needs.
16.5. Post-Procedure Communication
- Thank the patient for their cooperation.
- Provide instructions for post-procedure care.
- Inform them when and how they will receive their results.
17. Integrating Technology to Enhance Phlebotomy Practices
Technology plays an increasingly important role in modern phlebotomy practices, improving accuracy, efficiency, and patient safety.
17.1. Electronic Health Records (EHRs)
- Order Management: EHRs streamline the ordering process, reducing errors and improving communication between healthcare providers.
- Labeling: EHR-integrated labeling systems ensure accurate and consistent labeling of blood collection tubes.
- Documentation: EHRs provide a centralized location for documenting all aspects of the venipuncture procedure.
17.2. Barcode Scanning
- Patient Identification: Barcode scanning verifies patient identity, reducing the risk of misidentification.
- Specimen Tracking: Barcode scanning tracks blood samples throughout the laboratory workflow, ensuring accurate and timely processing.
17.3. Vein Visualization Devices
- Infrared Technology: Infrared vein finders enhance vein visibility, improving success rates for difficult venipunctures.
- Ultrasound Guidance: Ultrasound-guided venipuncture allows for precise needle placement, especially in patients with deep or fragile veins.
17.4. Automated Blood Collection Systems
- Robotic Phlebotomy: Robotic systems are being developed to automate the blood collection process, reducing human error and improving efficiency.
18. Understanding the Order of Draw: Minimizing Contamination
The order of draw is a crucial aspect of phlebotomy, designed to minimize the risk of cross-contamination between blood collection tubes. Following the correct order ensures accurate laboratory results.
18.1. Recommended Order of Draw
- Blood Culture Tubes: Drawn first to maintain sterility.
- Coagulation Tubes (Light Blue): Contain sodium citrate, which can affect other tests.
- Serum Tubes (Red, Gold, Tiger Top): Allow blood to clot before testing.
- Heparin Tubes (Green): Contain heparin, which can interfere with coagulation tests.
- EDTA Tubes (Lavender): Contain EDTA, which can affect electrolyte and enzyme measurements.
- Glycolytic Inhibitor Tubes (Gray): Contain sodium fluoride and potassium oxalate, used for glucose testing.
18.2. Rationale for the Order of Draw
- Additives: Different blood collection tubes contain various additives that can interfere with other tests if carried over.
- Contamination: Drawing tubes in the wrong order can lead to inaccurate results and potentially misdiagnosis.
18.3. Exceptions to the Order of Draw
- Syringe Draws: When using a syringe, the order of draw may need to be modified based on the specific tests ordered.
- Capillary Draws: Capillary blood collection has its own specific order of draw guidelines.
19. Quality Control Measures in Phlebotomy: Ensuring Accuracy
Quality control measures are essential for ensuring the accuracy and reliability of phlebotomy procedures.
19.1. Training and Competency
- Initial Training: Provide comprehensive training to all phlebotomists.
- Ongoing Education: Offer continuing education and competency assessments to maintain skills.
19.2. Equipment Maintenance
- Regular Inspections: Inspect equipment regularly for damage or malfunction.
- Proper Storage: Store supplies properly to maintain their integrity.
19.3. Procedure Standardization
- Written Protocols: Develop and follow standardized written protocols for all phlebotomy procedures.
- Adherence to Guidelines: Adhere to established guidelines for vein selection, needle insertion, and blood collection.
19.4. Monitoring and Auditing
- Error Tracking: Track and analyze errors to identify areas for improvement.
- Audits: Conduct regular audits of phlebotomy practices to ensure compliance with standards.
20. Resources for Nurses to Learn and Improve Phlebotomy Skills
There are numerous resources available to nurses seeking to learn or improve their phlebotomy skills:
- LEARNS.EDU.VN: Offers comprehensive online courses and resources on phlebotomy techniques and best practices. Contact us at 123 Education Way, Learnville, CA 90210, United States. Whatsapp: +1 555-555-1212.
- Hospital Training Programs: Many hospitals offer in-house training programs for nurses on phlebotomy.
- Community Colleges: Local community colleges often offer phlebotomy certification courses.
- Professional Organizations: Organizations such as the National Phlebotomy Association (NPA) and the American Society for Clinical Pathology (ASCP) provide educational resources and certification opportunities.
- Online Tutorials: Numerous online tutorials and videos demonstrate phlebotomy techniques.
- Textbooks: Several textbooks are available on phlebotomy and laboratory procedures.
- Mentorship: Seek guidance and mentorship from experienced nurses or phlebotomists.
By utilizing these resources and dedicating themselves to continuous learning, nurses can master the art of phlebotomy and provide exceptional care to their patients. Visit LEARNS.EDU.VN today to explore our phlebotomy resources and unlock your full potential!
 Nurse drawing blood from patient
Nurse drawing blood from patient
FAQ: Common Questions About Nurses and Blood Draws
How can nurses learn to draw blood effectively?
Nurses can learn to draw blood effectively through a combination of formal training, hands-on practice, and mentorship. Resources like LEARNS.EDU.VN offer comprehensive guides and courses.
What are the key techniques for successful blood draws by nurses?
Key techniques include proper vein selection, anchoring the vein, using the correct needle angle, and maintaining a steady hand during insertion.
How do nurses handle difficult patients during blood draws?
Nurses handle difficult patients by communicating clearly, explaining the procedure, addressing their fears, and using distraction techniques.
Why is the order of draw important for nurses drawing blood?
The order of draw is crucial to prevent cross-contamination of additives between tubes, ensuring accurate lab results.
Where can nurses find the best training resources for phlebotomy?
Nurses can find excellent training resources at LEARNS.EDU.VN, hospital training programs, community colleges, and professional organizations.
What are the common mistakes nurses make when drawing blood?
Common mistakes include improper vein selection, incorrect needle angle, failing to anchor the vein, and not inverting tubes properly.
How can nurses minimize patient discomfort during blood draws?
Nurses can minimize discomfort by using a gentle approach, applying topical anesthetics, and engaging the patient in conversation.
What are the legal considerations for nurses drawing blood?
Legal considerations include obtaining informed consent, maintaining patient confidentiality, and adhering to scope of practice guidelines.
How important is certification for nurses who draw blood?
Certification demonstrates competency and enhances credibility, promoting patient safety and increasing employability.
What role does technology play in helping nurses draw blood more efficiently?
Technology such as vein finders and EHRs improve vein visibility, streamline the process, reduce errors, and improve communication.
Ready to elevate your nursing skills and become a phlebotomy expert? Visit LEARNS.EDU.VN today to explore our comprehensive courses, resources, and expert guidance. Unlock your full potential and make a real difference in patient care. Contact us at 123 Education Way, Learnville, CA 90210, United States. Whatsapp: +1 555-555-1212. Invest in your future – start learning with learns.edu.vn now!
